Introduction
Porous tantalum (Ta) implants are becoming popular in orthopedics due to their outstanding properties as biomaterials. Known for their resistance to corrosion, compatibility with the body, ability to bond with bone, and conductivity, these implants are ideal for various uses, including joint replacements and spinal surgeries. Let’s learn about its features and uses in this article.
 [1]
[1]
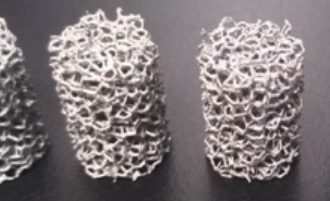
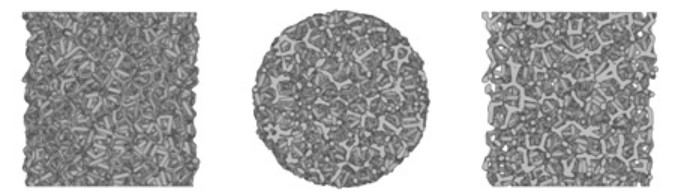
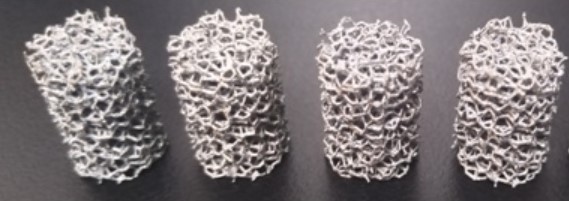
Structure of Porous Tantalum
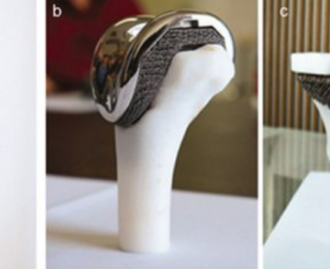
To appreciate the advantages of porous tantalum, we need to look at its structure. It features a honeycomb-like design with interconnected pores. This structure helps bone grow into the implant and allows calcium nodules to form, enhancing the implant’s connection with surrounding bone. The porous design is crucial, as it allows the implant to function similarly to natural bone. [1]
Related reading: Tantalum Metal Foam: An In-Depth Guide
Benefits of Porous Tantalum Implants
1. Mechanical Properties
Tantalum implants need to be strong and flexible to support joints and encourage bone healing. If an implant is too stiff, it can prevent new bone growth; if it’s too weak, it may not support the bone properly.
- Fatigue Resistance: Tantalum implants must endure repeated stresses without breaking. Research shows that porous tantalum has 8% greater fatigue strength than commercially pure titanium and 19% greater than titanium alloy Ti-6Al-4V, making it reliable for weight-bearing applications.
- Elastic Modulus: The implant’s stiffness should match that of human bone to avoid stress shielding, which can weaken the implant. Solid tantalum has a stiffness of 185 GPa, while porous tantalum ranges from 2.3 to 30 GPa. This range helps it mimic both hard (cortical) and soft (cancellous) bone, making it suitable for orthopedic use. [2]
2. Biocompatibility
Tantalum is also known for its excellent compatibility with the body. It resists corrosion and can form a protective oxide layer (Ta2O5), which helps develop a bone-like coating that promotes integration with bone.
3. Reduced Bacterial Adhesion
Porous tantalum minimizes bacterial adhesion, lowering the risk of infections after surgery. Its unique structure helps keep bacteria from settling on the implant, enhancing safety and effectiveness.
4. Induction of Osteogenesis
Additionally, tantalum encourages bone growth. Studies indicate that nanoparticles from tantalum implants can stimulate bone-forming cells (osteoblasts). This process is supported by specific biological pathways that help promote bone formation, making porous tantalum even more appealing for orthopedic use.
Applications and Clinical Cases
Porous tantalum implants are used in various clinical settings:
- Joint Replacement Surgeries: These implants have been successful in helping bones grow and bond with the implant. Patients who receive porous tantalum implants for hip and knee replacements often report better mobility and shorter recovery times compared to those with traditional implants.
- Spinal Surgery: In spinal procedures, porous tantalum implants provide crucial support and stability. Surgeons have found that these implants significantly reduce complications like migration or loosening. For example, in spinal fusion cases, porous tantalum has shown improved integration with the spine, leading to higher success rates and fewer revisions.
- Dental Applications: Porous tantalum is also making strides in dental implants. Studies show that patients with these implants often experience faster healing and greater satisfaction.
- Trauma Surgeries: In trauma cases, where promoting bone healing is critical, porous tantalum implants effectively distribute loads and support fracture healing.
Conclusion
In conclusion, porous tantalum implants represent a significant step forward in medical technology. Their unique combination of strength, compatibility with the body, and ability to promote bone growth makes them valuable for many applications. As research continues, the role of porous tantalum in improving patient care is likely to expand, leading to better treatments and enhanced quality of life for many patients. For more tantalum products, please check Advanced Refractory Metals (ARM).
Reference:
[1] Huang, G.; Pan, S.-T.; Qiu, J.-X. The Clinical Application of Porous Tantalum and Its New Development for Bone Tissue Engineering. Materials 2021, 14, 2647. https://doi.org/10.3390/ma14102647
[2] Wang X, Zhou K, Li Y, Xie H, Wang B. Preparation, modification, and clinical application of porous tantalum scaffolds. Front Bioeng Biotechnol. 2023 Apr 4;11:1127939. doi: 10.3389/fbioe.2023.1127939. PMID: 37082213; PMCID: PMC10110962.
Recent Comments